Part II Documentation & Medical Decision Making

Medical Record Documentation
In the 2020 PFS final rule, CMS finalized broad modifications to the medical record documentation requirements for physicians and certain NPPs. In this CY 2021 PFS final rule, they are clarifying that physicians and NPPs, including therapists, can review and verify documentation entered into the medical record by members of the medical team for their own services that are paid under the PFS. They are also clarifying that therapy students, and students of other disciplines, working under a physician or practitioner who furnishes and bills directly for their professional services to the Medicare program, may document in the record so long as the documentation is reviewed and verified (signed and dated) by the billing physician, practitioner, or therapist.
History and Exam
- No longer will be used to select the code level
- Medically appropriate history and exam
- Perform when clinically appropriate
- Number of systems reviewed will no longer apply
- Can be performed by staff and reviewed and signed off on by Providers
Chief Complaint
Providers not required to re-enter information or documentation by residents and the medical team
– Provider indicates “reviewed”.
– Document changes or additional information regarding encounter
Even though the amount of history or number of elements examined will not determine the overall E/M level of service, a history and physical examination will still need to be performed if medically appropriate and of course documented.
Documentation Requirements when Coding for Time:
– Documentation must clearly indicate nature of services performed
- “I spent an hour on the phone after patient's appointment” is not sufficient
- Documentation must indicate amount of time for these separately reported services was not included in total time for the E/M level selection
- If reporting both an E/M service by time and minor procedure documenting “total patient care time 30 min” is not sufficient
- Documentation must support medical necessity of time spent on patient encounter
- If a 50 min visit is documented and billed as 99215 with a diagnosis of cough with no other information may not be sufficient
Evaluation & Management Codes (E&M codes)
New Patient
(99201 has been deleted. To report, use 99202)
99202 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and straightforward medical decision making.
When using time for code selection, 15-29 minutes of total time is spent on the date of the encounter.
99203 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making.
When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter.
99204 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making.
When using time for code selection, 45-59 minutes of total time is spent on the date of the encounter.
99205 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and high level of medical decision making.
When using time for code selection, 60-74 minutes of total time is spent on the date of the encounter.
(For services 75 minutes or longer, see Prolonged Services 99XXX)
Established Patient
99211 Office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician or other qualified health care professional. Usually, the presenting problem(s) are minimal.
99212 Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and straightforward medical decision making. When using time for code selection, 10-19 minutes of total time is spent on the date of the encounter.
99213 Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 20-29 minutes of total time is spent on the date of the encounter.
99214 Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using time for code selection, 30-39 minutes of total time is spent on the date of the encounter.
99215 Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using time for code selection, 40-54 minutes of total time is spent on the date of the encounter. (For services 55 minutes or longer, see Prolonged Services 99XXX)
The table below indicates the time for the outpatient E/M codes when coding is based on time.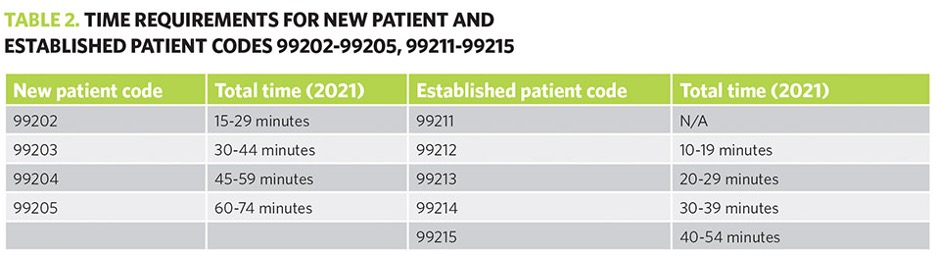
KEY TAKEAWAYS
- Changes apply only to office and other outpatient E/M services (99202-99215)
- CPT code 99201 will be deleted due to low utilization
- Providers will select the E/M code based only on the level of medical decision making (MDM) or total time
- History and examination will no longer be significant in determining the level of service
- Total time is defined as “total time spent on the day of the encounter”
- Revisions to the MDM elements for codes 99202–99215:
- “Number of Diagnoses or Management Options” will change to “Number and Complexity of Problems Addressed”
- “Amount and/or Complexity of Data to be Reviewed” will change to “Amount and/or Complexity of Data to be Reviewed and Analyzed”
- “Risk of Complications and/or Morbidity or Mortality” will change to “Risk of Complications and/or Morbidity or Mortality of Patient Management”
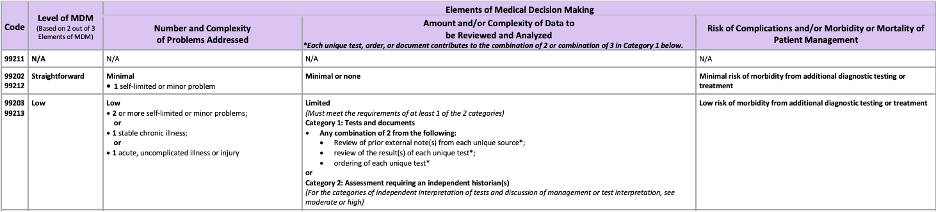
A Deeper Dive into Medical Decision Making (MDM)

Modifications to criteria for MDM:
– CMS Table of Risk used as foundation to create Level of Medical Decision-Making Table
- Removed ambiguous terms (e.g., "mild”) defined previously ambiguous concepts (e.g., acute or chronic illness with systemic symptoms”)
- Provides a guide to assist in selecting level of MDM used for office or other outpatient E/M services
- Includes four levels of MDM (unchanged from current levels of MDM)
- Straightforward
- Low
• Moderate
• High
MDM Table
MDM 2020 MDM Effective 1/1/2021
Number of Diagnosis or Number of Complexity of Problems Addressed at the Management Options. Encounter
Amount and/or Complexity of Amount and/or Complexity of Data to be Reviewed and Data to be Reviewed Analyzed
Risk of Complications and/or Risk of Complications and/or Morbidity or Mortality of Mortality Morbidity of Mortality. Patient Management
MDM Elements
- Elements include:
- The number and complexity of problems addressed in the encounter, meaning it will no longer be necessary to document every diagnosis a patient has received— just those being addressed during that visit.
- The amount or complexity of data to be reviewed and analyzed. This reduces cut-and-paste, not requiring physicians to enter “voluminous,” repetitive test data that is irrelevant or ancillary to the purpose of the visit.
- Risk of complications or morbidity of patient management. can now include social determinants of health and reasons behind decisions not to admit a patient or intervene in some way.
MDM: Number and Complexity of Problem(s) Addressed at Encounter
Clinically Relevant
- Straightforward – Self-limited
- Low
– Stable, uncomplicated, single problem - Moderate
– Multiple problems or significantly ill - High
– Very ill
MDM: Amount and/or Complexity of Data to be Reviewed and Analyzed
Straightforward – Minimal or none
- Low (one category)
– Two documents or independent historian - Moderate (one category only)
– Count: Three items between documents and independent historian; or
– Interpret; or
– Confer
- High (two categories)
– Same concepts as moderate
MDM Data
Data is divided into three categories:
- Tests, documents, orders, or independent historian(s)–each unique test
- Independent interpretation of tests not reported separately
- Discussion of management/test interpretation with external physician/other QHP appropriate source (not reported separately)
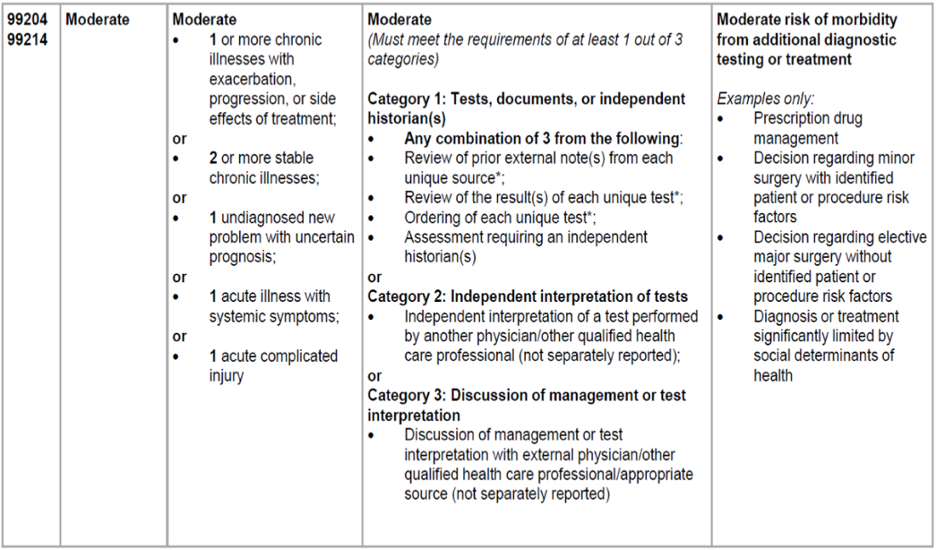
MDM: Risk of Complications and/or Morbidity or Mortality of Patient Management
Straightforward– Minimal risk from treatment (includes no treatment) or
- Low
– Low risk (very low risk of severity problems), minimal consent/discussion
- Moderate
– Typical review with patient/surrogate, obtain consent and monitor/or management of complex social factors
- High
– Need to discuss high risk problems that could happen for which physician or other QHPs will watch or monitor
Made at the visit, associated with patient's problem(s), treatment(s)
– Includes possible management options selected and those not selected
– Addresses risks associated with social determinants of health
MDM Example
- patient visits cardiologist for appointment complaining of occasional chest discomfort during exercise. Patient has history of hypertension and high cholesterol which are currently under control with prescribed medications. Physician completes examining and assessing the patients and determines patient needs a cardiovascular stress test. Its ordered and performed that same day by same provider
- Which E/M code should be reported? 99214
- With modifier 25
- And the 93015 for the stress test
MDM Table:
See Part III for a Deeper Dive into Prolonged Services Changes for 2021