MGMA STAT
Some health plans and their contracted payment vendors have sought to take advantage of physician practices by forcing them to pay fees to receive their payments for medical services via Electronic Funds Transfer (EFT). These transaction fees typically range from 2-5% of the total medical services payment. As part of an effort in the Affordable Care Act to decrease healthcare administrative inefficiencies, the Centers for Medicare & Medicaid Services (CMS) mandated a standard EFT transaction and supporting operating rules and since 2014 health plans are required to offer EFT should providers request it.
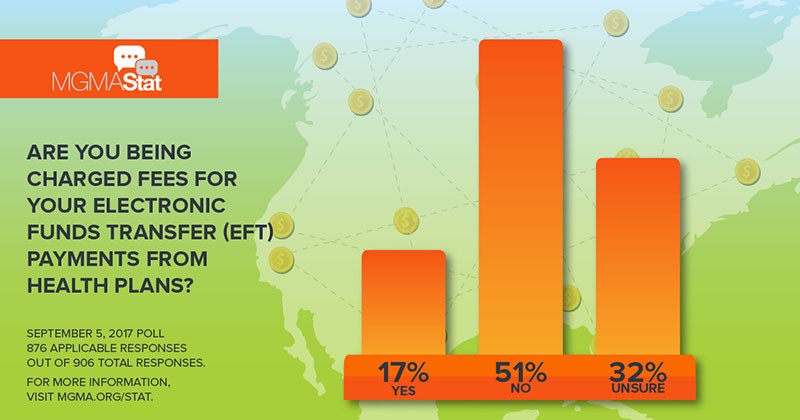
A Sept. 5 MGMA Stat poll, with responses from more than 900 individuals, found that 17% of respondents indicated that their EFT payments from health plans came with a fee, with 50% saying there was no fee attached to the transaction. More than 32% indicated that they were unsure. Of those who responded yes to receiving fees for EFT payments, almost 60% stated that these health plans use a third-party payment vendor. Medical groups are forced to pay these EFT fees as CMS has yet to issue guidance preventing health plans and payment vendors from charging these fees.
“Even though health plans save money not printing and mailing paper checks, some bad actors are fleecing physician groups by charging them to simply receive an electronic paycheck,” stated Anders Gilberg, MGMA Senior Vice President, Government Affairs. “It is critical that CMS issue long-overdue guidance explicitly prohibiting this practice.”
The savings and benefits related to use of EFT for business and consumer payments are well established. Not only do health insurers save millions of dollars sending payments via EFT, for practices, the most common savings are in the ability to automate the reassociation of the electronic payment with the Electronic Remittance Advice, as well as savings in staff time to manually process and deposit paper checks. Beyond the material and administrative time savings for all sides, the time and resources that physician practices spend on billing and related tasks are better spent on delivering healthcare to patients.